Translate this page into:
Psychosocial Support after Laryngectomy of a Patient with Laryngeal Squamous Cell Carcinoma – A Case Study

*Corresponding author: Sucharita Chatterjee, Department of Oncology, Command Hospital (Eastern Command), Kolkata, West Bengal, India. s.chattopadhyay4991@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chatterjee S, Pathak A, Bandyopadhyay A, Pandya T, Singh VK. Psychosocial support after laryngectomy of a patient with laryngeal squamous cell carcinoma – A case study. Indian Cancer Awareness J 2022;1:24-6.
Abstract
A case study of a 70-year-old male diagnosed with laryngeal squamous cell carcinoma, having difficulty in accepting the situation after total laryngectomy along with multiple stressors. A short-term psychological intervention was planned and implemented in the indoor patient department. The outcome of the intervention reflected an improvement in the mental health of the patient and gradual acceptance of the situation. Further researches are needed in this area to generalise the efficacy of the intervention.
Keywords
Psychological intervention
Laryngectomy
Carcinoma glottis
Mental health
INTRODUCTION
Laryngeal cancer is the second leading cause of cancer in males in the age group of 70–74 in comparison to other head-and-neck cancers in the same age band in India as reported by National Cancer Registry Programme 2012–2016.[1] Laryngectomy is the surgical removal of the larynx and is an established, effective treatment for locally advanced laryngeal cancer.[2] However, it markedly alters the patient’s post-operative quality of life and increases the risk of psychological morbidity.[3,4] The present case study is mainly focusing on the psychosocial aspects of the patient and short-term psychological intervention after the surgery.
CASE REPORT
A 70-year-old male hailing from an urban area of West Bengal was diagnosed with carcinoma glottis and was on radiation therapy during the pandemic situation. After taking several numbers of radiations, it was observed that his voice tone was gradually reducing. His younger son who was involved in his treatment process and used to take care of him died of COVID during his ongoing treatment process. Doctors recommended a total laryngectomy within a few months of his son’s death. Initially, he was completely against this surgery. However, pre-operative counselling by doctors and family members’ support encouraged and motivated him to comply with the treatment process.
The individual was a boxing champion and worked as a coach for several renowned boxing clubs as reported by the patient. He used to excel in his occupational and social life most of the time. However, since the beginning, he has had an anger issue, difficulty in accepting failure, and an increased need for perfection as reported by the informant. A gradual change in his behavioural pattern such as sadness, irritability, and anger outburst was reported to be observed often and aggravated after the surgery (total laryngectomy) [Figure 1 – Case Conceptualisation].
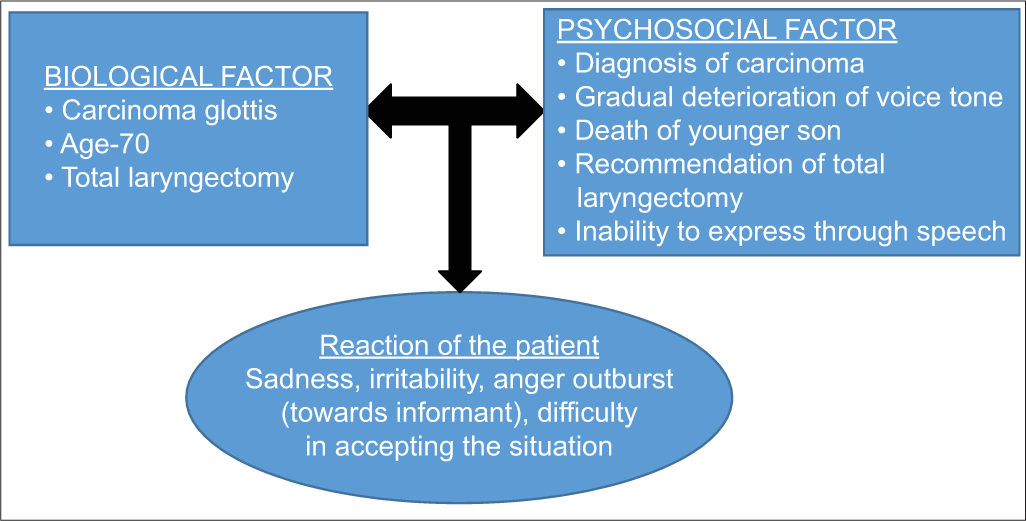
- Case conceptualisation through biopsychosocial model.
Psychological intervention planning and implementation
The locus of the intervention was planned in the indoor patient department. Visual analogue scale (10 points scale) was used to measure subjective unit of distress (SUD) to assess the progress of the intervention. Thrice a week session in the initial phase was considered necessary after discussion with the client and his informant. Six sessions could be taken before the discharge of the patient. At the beginning of the intervention, SUD was assessed and found to be 9. Therapeutic targets were selected to reduce the SUD and change the appraisal of the situation by addressing automatic thoughts through cognitive restructuring. Communication with the patient was planned to be done through writing from both sides (patient and therapist).
In the first session, the client was refused to communicate on his own but wanted to continue the process through an informant (family member). Psychoeducation was done about the reactions of the patient, causes, prognosis, and the treatment mode – pharmacotherapy and psychotherapy. A family member was ventilating about the journey of illness and their son’s death. Ventilation was encouraged through active listening, distress was validated and normalised. A family member was given general guidance regarding the reaction of the patient. In the second session, he was agreed to communicate through writing. He ventilated regarding his unwillingness for the surgery, his treatment process, and inability to express himself through voice. Ventilation was encouraged; distress was validated and normalised through writing only. He also ventilated through tears along with the printed letters. He was also expressing his achievements and passion for boxing. At the end of the session, SUD was 7 and an assignment was given to write on his achievements and passion.
In the third session, the patient reported that he was doing better through gestures and forgot to write the assignment. In the fourth session, he showed the assignment, wrote one page about himself, and the ending line of the writing communicated that he was not motivated to do the assignment. His effort was appreciated and appraisal of the situation was addressed. At the end of the session, SUD was 6. No further assignment was given.
In the fifth session, the patient reported that he was doing better through gestures and the informant also communicated the same. In the sixth session, the patient himself wrote two pages about his life and passion and wanted the therapist to read them. The writing also reflected the hope about the treatment process and the gradual acceptance of the situation. His effort was appreciated and was encouraged to maintain hope. At the end of the session, SUD was 3 [Figure 2 – Subjective Unit of Distress Across Sessions].

- Subjective unit of distress.
CONCLUSION
This case study illustrated that how psychological intervention helps in the improvement of the patient’s mental health after laryngectomy, makes the journey of acceptance easier for the patient, and helps to cope with the situation in a better way. However, it is difficult to generalise the application of the intervention based on a single-case study. Future research in this area would shed more light on the efficacy of the intervention.
Acknowledgement
I would like to convey my heartfelt gratitude to Lt Col. Dr. Abhishek Pathak, Medical Oncologist, Command Hospital (Eastern Command) for constant encouragement, support, and guidance. I am thankful to the patient and his family member for their cooperation throughout the intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Locally advanced laryngeal cancer: Total laryngectomy or primary non-surgical treatment? Oncol Lett. 2018;15:6701-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mental disorders and psychosocial support during the first year after total laryngectomy: A prospective cohort study. Clin Otolaryngol. 2013;38:494-501.
- [CrossRef] [PubMed] [Google Scholar]
- The psychosocial impact of a laryngectomy. J Psychosoc Oncol. 1991;9:37-58.
- [CrossRef] [Google Scholar]






