Translate this page into:
Inflammatory Myofibroblastic Tumour Presenting as Posterior Mediastinal Mass in a Child – A Rare Case Report

*Corresponding author: Thirunavukkarasu Arun Babu, Department of Pediatrics, All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India. babuarun@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Balakrishnan P, Arun Babu T. Inflammatory myofibroblastic tumour presenting as posterior mediastinal mass in a child – A rare case report. Indian Cancer Awareness J. 2023;2:60-2. doi: 10.25259/ICAJ_10_2023
Abstract
Posterior mediastinal tumours in children are difficult to diagnose due to non-specific clinical symptoms. Most of them are neurogenic in origin. However, large pulmonary neoplasms in children may also present as posterior mediastinal masses and may be misinterpreted as neurogenic tumour. We report a case of 6-year female child with recurrent vomiting who had inflammatory myofibroblastic tumour of the right lung which presented as posterior mediastinal mass on computed tomography.
Keywords
Children
Posterior mediastinum
Inflammatory myofibroblastic tumour
Vomiting
INTRODUCTION
Inflammatory myofibroblastic tumour (IMT), pleuropulmonary blastoma and carcinoid tumour are the common primary neoplasms of lung in children.
IMTs constitute 0.04–1% among all pulmonary neoplasms and are mostly seen in children and young adults.[1]
The pre-operative diagnosis is difficult due to clinical heterogeneity and non-specific radiological findings. Definitive diagnosis of IMTs is achieved only by pathological examination of mass. We report a case of 6-year female child with recurrent vomiting who had IMT of the right lung which presented as posterior mediastinal mass on computed tomography.
CASE REPORT
A 13-year-old female child presented to paediatric outpatient department with complaints of recurrent vomiting for 1 week and severe dysphagia, intermittent chest pain and loss of weight for 1 month. Vomitus was bile stained, non-blood stained, and contained food particles. Dysphagia was severe and was even for liquids. Chest pain was in the right parasternal region, intermittent associated with vomiting and non-radiating. There was no history of fever, trauma, diarrhoea and mass per abdomen, haematemesis and breathlessness. There was no significant past history and family history.
General physical examination and systemic examination were normal except for pallor. Complete haemogram showed microcytic hypochromic anaemia of moderated degree with neutrophilic leucocytosis. Her erythrocyte sedimentation rate (ESR) was 70 mm/h. C-reactive protein was positive. X-ray of abdomen erect posture and ultrasonogram of abdomen, sputum smear for acid-fast bacilli and electrocardiogram were unremarkable.
She was treated with antiemetics and antacids considering probable diagnosis of acute gastritis. Vomiting was recurrent and refractory to empirical therapy. Chest X-ray showed mediastinal widening with clear lung fields. High-resolution computed tomography showed large lobulated heterogenous mass measuring 70 × 40 mm occupying posterior mediastinum with peripheral calcifications. The mass was compressing oesophagus with proximal dilatation of oesophagus. The mass also abutted aorta with loss of fat planes [Figures 1a and b].
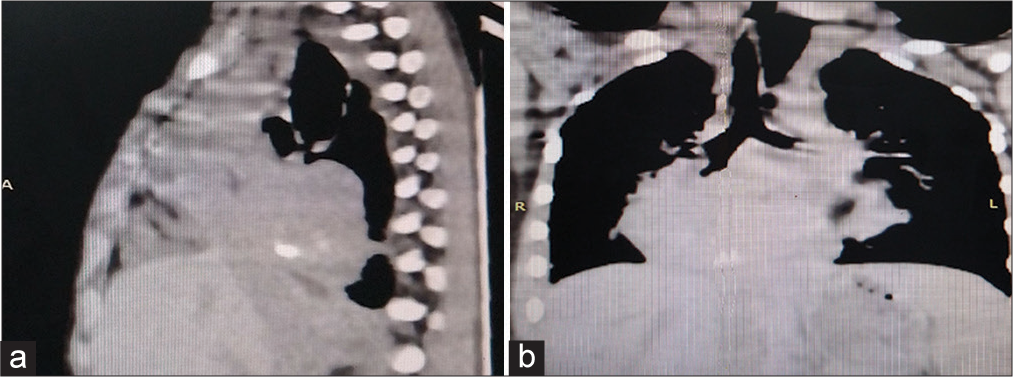
- (a and b) High-resolution computed tomography of chest of child showing large lobulated heterogenous mass of 70 × 40 mm with calcifications in posterior mediastinum (coronal view and sagittal view).
With radiological features, malignant neoplasm occupying posterior mediastinum probably neuroblastoma was considered as pre-operative diagnosis. Magnetic resonance imaging (MRI) brain was normal.
Under general anaesthesia, right thoracotomy through right posterolateral incision was done. Intraoperatively, the mass was arising from middle and lower lobes of right lung. It was enclosing distal thoracic oesophagus and infiltrating posterior thoracic wall. Right middle and lower lobectomy with partial excision of mass were done. The part of mass encircling the distal oesophagus and posterior thoracic duct could not be excised. The post-operative period was uneventful.
Grossly partial pneumonectomy specimen was 7 × 5 × 2 cm and 100 g with a well-defined mass of 6 × 4 × 2 cm. Cut surface of mass was solid, homogenous and grey white with peripheral normal appearing lung parenchyma [Figure 2a]. Histopathological examination showed lung parenchyma with a tumour in the parabronchial region composed of compact bundles and fascicles of spindle cells with abundant eosinophilic cytoplasm and elongated vesicular nucleus, fine granular chromatin with prominent nucleoli [Figure 2b]. The was no nuclear pleomorphism, nuclear atypia or atypical mitotic figures in tumour cells. In the background, there were fibrous tissue and dense inflammatory cell collections such as plasma cells, lymphocytes, macrophages and eosinophils [Figure 2c]. There was no infiltration of bronchi and pleura by tumour. Immunohistochemical analysis of tumour showed positivity for vimentin, desmin and anaplastic lymphoma kinase (ALK) markers. Correlating clinical, radiological and pathological findings, the diagnosis of IMT of the right lung was made.

- (a) Gross photograph of lobectomy specimen showing well-defined homogenous grey white solid mass with peripheral firm grey tan lung parenchyma. (b) Microphotograph showing bronchus with adjacent tumour composed of fascicles of spindle cells and inflammatory cells (H and E stain, ×100). (c) Microphotograph showing tumour composed of fascicles of spindle cells with abundant eosinophilic cytoplasm, elongated vesicular nucleus with dense collections of plasma cells and lymphocytes (H and E stain, ×400).
After 1 month of initial surgery, child again presented with intermittent fever, vomiting and dysphagia for liquids. Barium swallow radiogram showed dilated upper and middle thoracic oesophagus with barium trapping and tapering of distal oesophagus with smooth borders [Figure 3]. Computed tomography chest showed post lobectomy status of the right lung and residual mass compressing oesophagus. There was no evidence of metastasis investigated by MRI abdomen and brain.

- Post-operative barium swallow radiogram of child showed dilated upper and middle thoracic oesophagus with barium trapping and tapering of distal oesophagus with smooth borders.
The child was referred to higher centre for chemotherapy and was lost to follow-up.
DISCUSSION
Posterior mediastinal tumours in children may be neuroblastoma, ganglioneuroblastoma, ganglioneuroma, pulmonary neoplasms such as pleuropulmonary neuroblastoma, carcinoid tumour and chest wall neoplasm like Askin’s tumour may also present as posterior mediastinal mass.[2]
IMTs present as solitary nodules in subpleural location, peripheral lung parenchyma or around hilum in radiograph. In only 5% of cases, lung IMTs extend towards mediastinum, diaphragm, pleura or chest wall.[3] Mediastinal neuroblastoma was considered as probable radiological diagnosis in the present case.
When the posterior mediastinal mass is large with features of local invasion and systemic inflammation such as high ESR, C-reactive protein positive, leucocytosis and the possibility of IMT must be suspected as in present case.
A case of IMT involving left upper lobe presented as posterior mediastinal tumour in 6-year old female child was reported.[4] In present case, the tumour involved middle and lower lobes of right lung.
In the literature, presentation of IMT with vomiting was rarely reported. In present case, vomiting was due to compression of distal oesophagus by large mass which misguided us to consider gastrointestinal lesions as first clinical diagnosis. In children, IMTs present with symptoms not only pertaining to structure they arise but also to structures they invade and compress.
When IMTs are suspected, complete surgical resection is recommended due to risk of sarcomatous transformation, metastasis and recurrence. In present case, complete surgical resection could not be achieved due to encirclement of oesophagus and aorta by tumour. Hence, prolonged follow-up of cases is also advised for the same.[3]
Pre-operative chemotherapy with crizotinib in large ALK positive tumour is recommended.[5]
In present case, as the diagnosis of IMT was made in postoperative period, preoperative chemotherapy could not be given. The child was referred to higher centre for postoperative chemotherapy.
CONCLUSION
Large IMT of lung can present as posterior mediastinal mass. It mimics malignancy as it has nonspecific clinical, and radiological findings and locally invasive nature. Clinicians must be aware of its malignant potential, and hence, complete surgical resection must be done. Histopathology and immunohistochemistry help in definitive diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Inflammatory myofibroblastic tumours of the thorax: Radiologic and clinicopathological correlation. Indian J Radiol Imaging. 2020;30:266-72.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant pulmonary and mediastinal tumors in children: Differential diagnoses. Cancer Imaging. 2010;10:S35-41.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory myofibroblastic tumor of the lung: A rare entity. Respir Med Case Rep. 2020;31:101287.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior mediastinal myofibroblastic tumour in a 6-year-old. J Pediatr Surg Case Rep. 2020;61:101575.
- [CrossRef] [Google Scholar]
- Clinical characteristics and prognosis of pulmonary inflammatory myofibroblastic tumor: An over 10-year retrospective analysis. Pediatr Investig. 2020;4:192-7.
- [CrossRef] [PubMed] [Google Scholar]