Translate this page into:
Why are You Late? A Descriptive Study of Delay in Treatment Seeking among Patients of Carcinoma Breast Presenting to a Tertiary Care Hospital in South India

*Corresponding author: Gomathi Shankar, Department of General Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. drgomathishankar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patta MK, Shankar G, Ahmed FM. Why are You Late? A Descriptive Study of Delay in Treatment Seeking among Patients of Carcinoma Breast Presenting to a Tertiary Care Hospital in South India. Indian Cancer Awareness J. 2024;3:9-16. doi: 10.25259/ICAJ_4_2024
Abstract
Objectives:
The objectives of this study were as follows: Primary: To estimate the proportion of breast cancer patients with delay in presentation. Secondary: To assess the reasons for delay in presentation among patients with breast cancer. To identify the sociodemographic and clinical characteristics associated with delayed presentation among patients with breast cancer.
Materials and Methods:
We conducted a hospital-based descriptive study at a tertiary care hospital- Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), from a period of January 2016 to June 2016. The participants were interviewed at the time of their hospital visit with a standardised questionnaire after obtaining informed consent. The patients were asked to recall the time interval between the first recognition of symptoms and the first medical consultation. A duration of >3 months was considered a patient delay. The patient reported the first symptom, and the symptoms at presentation were noted. Through clinical examination of the breasts, axilla and other systems was performed, and the positive clinical features were recorded.
Results:
A total of 126 women were included in the study. Out of 126 patients, 37 patients (29.4%) presented to healthcare personnel within 3 months of identifying their symptoms, and 89 patients (70.6%) presented later than 3 months. The mean duration of delay is 171.5 days, with a standard deviation of 229.45 and a median delay being 120 days. The most common cause for delay was due to the patient’s perception that the lump was harmless or temporary. The average time taken by the patients to present to JIPMER for definitive management of breast cancer after visiting a local physician was a median of 25 days and a mean of 48.77 days. The time taken for confirmation of diagnosis from the time of presentation to JIPMER was a median duration of 13 days and a mean duration of 16.58 days with a standard deviation of 12.31. About 90% of the patients had their diagnosis confirmed within 1 month.
Conclusion:
In our study, the proportion of delayed presentation among breast cancer patients was found to be 70.6%. Patients from rural areas and with lower educational status were found to have a higher incidence of delayed presentation. Lack of awareness of breast cancer symptoms and their misinterpretation as harmless, temporary and benign are the main reasons for delayed presentation. Patients who practised breast self-examination presented earlier. Further studies with a larger sample will help in identifying the other sociodemographic and clinical characteristics responsible for delayed presentation.
Keywords
Breast cancer
Delay
Patient delay
System delay
Provider delay
INTRODUCTION
Breast cancer is the most common cause of cancer-related mortality among women.[1] The delay in the presentation of the patient to the healthcare system and the delay in diagnosing and treating the condition thereafter worsen the prognosis of the patient.[2] Majority of the patients in developing countries present at an advanced stage compared to developed countries. Hence, even though the incidence of breast cancer is higher in the developed countries, the mortality rates are higher in the developing countries.[1,3,4]
The reasons for this delay can be divided into patient delay, provider delay and system delay. Patient delay is the time interval between identification of symptoms by the patient to seek a health-care practitioner’s advice. Provider delay is the time from the first visit to a healthcare provider and referral for diagnostic tests or specialist assessment. System delay is the time between referral and definitive diagnosis and treatment.[5-7] Each of these delays has multiple factors influencing them. Some of the important factors influencing patient delay are recognition of symptoms and their interpretation, psychological factors and sociodemographic and cultural factors. Provider delay could be due to misdiagnosis, inadequate examination, or ignoring patient symptoms, whereas system delay is the time taken for investigations and administrative delay for follow-up.[8,9] These factors need to be studied in detail, and the major causes of delay need to be identified to tailor the solution.
The past studies investigating the causes of delay show that the reasons for delay are heavily based on the social, economic, educational and cultural aspects of the population being studied, and the results from one region are not generalisable. According to a systematic review of Indian studies on the barriers to breast cancer care in developing countries, including thirteen studies, poverty constitutes the most important barrier contributing to delayed patient presentation. Conditions of poverty, including lower-income status, rural residency, lower educational level and lack of access to healthcare systems, were found to be associated with delayed presentation.[10] The association between marital status and family history on patient delay was not consistent in various studies. The delay was more among widowed or divorced women, according to some studies[11,12] whereas it was more among married women according to another study.[13] One study showed increased delay in case of positive family history[11] whereas another study showed patients with positive family history presenting early.[13]
The results of the past studies are conflicting. In addition, there has been only one South Indian study on the subject, and it was a retrospective database-based study.[11] Ours was a prospective study which aimed at identifying the reasons for delayed presentation of breast cancer among the South Indian population presenting to a tertiary care centre.
Objectives
The objectives of this were as follows:
Primary
To estimate the proportion of breast cancer patients with delay in presentation.
Secondary
To assess the reasons for delay in presentation among patients with breast cancer
To identify the sociodemographic and clinical characteristics associated with delayed presentation among patients with breast cancer.
MATERIALS AND METHODS
We conducted a hospital-based descriptive study at a tertiary care hospital – Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), from a period of January 2016 to June 2016. All patients with breast cancer presenting to the surgical outpatient department were screened for eligibility. The patients with histologically proven carcinoma were included in the study. Women with recurrent breast cancers, past or present history of other cancers and breast cancer diagnosed by screening were excluded from the study. The participants were interviewed at the time of their hospital visit with a standardised questionnaire after obtaining informed consent.
The patients were asked to recall the time interval between the first recognition of symptoms and the first medical consultation. A duration of >3 months was considered a patient delay. The sociodemographic data of the patient was collected, including age, education, monthly family income, occupation, marital status, and residence. Clinical variables- family history of breast cancer, history of benign breast disease, parity, menopausal status, comorbidities and use of alternative medicine were recorded. Whether the patient performed breast self-examination or examination by a health-care provider was noted.
The first symptom, as reported by the patient, and the symptoms at presentation were noted. A thorough clinical examination of the breasts, axilla, and other systems was performed, and positive clinical features were recorded.
The study was based on recall by the patients. To overcome this, any patient who doubted whether the symptoms had been present for 3 months or longer was given the benefit of the doubt and placed in the <3 months group.
Sample size calculation
The sample size was calculated using an open-source calculator, OpenEpi, Version 3, for a 95% confidence interval (CI) and 5% precision, with an expected proportion of delayed presentation of 61.6%. We required a sample size of 121, and allowing a 5% dropout rate, the final sample size was 126.
Statistical analysis
Data were entered into a Microsoft Excel spreadsheet and imported to EpiData analysis software for analysis. Continuous variables were summarised as mean and standard deviations. Categorical variables were summarised as percentages. The outcome variable delayed presentation to health facility was summarised as a percentage with 95% confidence levels. Reasons for delay in reaching health facility were summarised as percentages.
To assess the possible association of sociodemographic and clinical characteristics with delayed presentation, we used the Chi-square test to assess the association of categorical predictors with the outcome. To assess the independent effect of variables (after adjusting for confounding effect), we performed multivariate analysis using log-binomial regression to calculate adjusted prevalence ratios with 95% CIs. Those variables which were significant in univariate analysis at P < 0.2 were included in the multivariate model. P < 0.05 was considered statistically significant for all analyses.
RESULTS
A total of 128 women were included in the study. Two women did not show malignancy in the histopathological report after an initial clinical diagnosis of breast cancer and were excluded from the study.
Sociodemographic distribution
The mean age of patients included in the study was 48.57, with a standard deviation of 11.24, ranging from 26 years to 88 years. About 58% of patients were from urban residences. About 47.6% of the patients were illiterates, 26.2% were of primary or middle class, and 26.2% belonged to high school and above educational status. About 48.4% of them were daily wage labourers, 47.6% were housewives, and 4% were employed. About 24.6% of them belonged to the monthly income level of <10000, whereas 75.4% of them were in the income range of 10,000 and above. All of them were married, 92.1% were living with a spouse, and 7.9% of them were widows.
Symptoms
Almost all patients had a painless breast lump as their first symptom. Only one patient had pain as her first symptom. At presentation to the healthcare provider, 36.5% of patients had pain, 4% had developed nipple discharge, 3.2% had nipple distortion, 7.1% had an ulcer, and 3.2% had axillary swelling.
Among 126 patients, 2 (1.6%) patients had a positive family history of breast cancer. Three (2.4%) patients had a history of benign breast disease. Only 3 (2.4%) patients were nulliparous. About 28.6% of patients had associated comorbid illness. About 39.7% of patients were premenopausal. Breast self-examination was practised by 16 patients, accounting for 12.7%. None of the patients had had clinical breast examination by professional health-care personnel during their previous hospital visits. About 7.9% of the patients were provided with information on breast cancer during their lifetime.
The oncological details of the study population are represented in Graph 1 and Table 1.
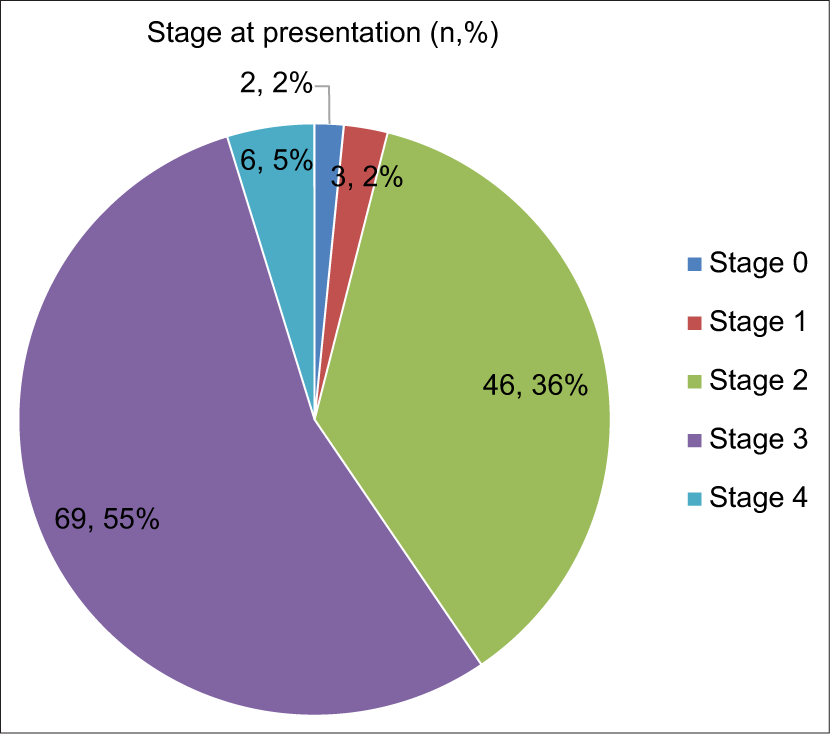
- Stage at presentation.
| Histopathological type | Frequency (n, %) |
|---|---|
| Infiltrating ductal carcinoma | 120 (95.2) |
| Ductal carcinoma in situ | 2 (1.6) |
| Adenoid cystic carcinoma | 1 (0.8) |
| Colloid carcinoma | 1 (0.8) |
| Invasive micropapillary carcinoma | 1 (0.8) |
| Metaplastic breast cancer | 1 (0.8) |
| Total | 126 (100.0) |
Patient delay
Out of 126 patients, 37 patients (29.4%) presented to healthcare personnel within 3 months of identifying their symptoms, and 89 patients (70.6%) presented later than3 months. The mean duration of delay was 171.5 days with a standard deviation of 229.45, and the median delay was 120 days, with the time interval ranging from 3 days to 5 years. The demographic distribution of the patients with and without delay is detailed in Table 2. The results of the multivariate analysis for the significant variables are presented in Table 3.
| Delay <3 months n (%) | Delay ≥3 months n (%) | P-value | |
|---|---|---|---|
| Age | |||
| <34 | 4 (10.8) | 8 (9) | 0.90 |
| 35–44 | 11 (29.7) | 21 (23.6) | |
| 45–54 | 11 (29.7) | 33 (37.1) | |
| 55–64 | 8 (21.6) | 18 (20.2) | |
| >65 | 3 (8.1) | 9 (10.1) | |
| Residence | |||
| Rural | 8 (15.4) | 44 (84.6) | 0.003 |
| Urban | 29 (39.2) | 45 (60.8) | |
| Education | |||
| Illiterate | 10 (16.7) | 50 (83.3) | 0.001 |
| Primary/middle | 10 (30.3) | 23 (69.7) | |
| High school | 17 (51.5) | 16 (48.5) | |
| Occupation | |||
| Labourer | 15 (24.6) | 46 (75.4) | 0.213 |
| Housewife | 19 (31.7) | 41 (68.3) | |
| Employed | 3 (60) | 2 (40) | |
| Income | |||
| <10000 | 6 (19.4) | 25 (80.6) | 0.158 |
| 10,000 and above | 31 (32.6) | 64 (67.4) | |
| Marital status | |||
| Married | 33 (28.4) | 83 (71.6) | 0.44 |
| Widowed | 4 (40) | 6 (60) | |
| Comorbid illness | |||
| Absent | 29 (32.2) | 61 (61.8) | |
| Present | 8 (22.2) | 28 (77.8) | |
| Breast self-examination | |||
| Not done | 26 (23.6) | 84 (76.4) | 0.0002 |
| Done | 11 (68.3) | 5 (31.3) | |
| Breast cancer information | |||
| Not received | 30 (25.9) | 86 (74.1) | |
| Received | 7 (70) | 3 (30) | |
| Stage | |||
| 0 | 1 (2.7) | 1 (1.1) | 0.001 |
| 1 | 2 (5.4) | 1 (1.1) | |
| 2 | 2 (75.7) | 18 (20.2) | |
| 3 | 6 (16.2) | 63 (70.8) | |
| 4 | 0 (0) | 6 (6.7) |
| Delay <3 months n (%) | Delay ≥3 months n (%) | Unadjusted prevalence ratio (95% CI) | Adjusted prevalence ratio (95% CI) | |
|---|---|---|---|---|
| Residence | ||||
| Rural | 8 (15.4) | 44 (84.6) | 1.4 (1.1–1.7) | 1.1 (0.9–1.4) |
| Urban | 29 (39.2) | 45 (60.8) | Ref | |
| Education | ||||
| Illiterate | 10 (16.7) | 50 (83.3) | 1.7 (1.2–2.5) | 1.4 (0.9–2.1) |
| Primary/middle | 10 (30.3) | 23 (69.7) | 1.4 (0.9–2.2) | 1.3 (0.8–1.9) |
| High school | 17 (51.5) | 16 (48.5) | Ref | |
| Occupation | ||||
| Labourer | 15 (24.6) | 46 (75.4) | 1.9 (0.6–5.6) | 1.1 (0.3–4.1) |
| Housewife | 19 (31.7) | 41 (68.3) | 1.7 (0.6–5.1) | 1.1 (0.3–3.9) |
| Employed | 3 (60) | 2 (40) | Ref | |
| Income | ||||
| <10,000 | 6 (19.4) | 25 (80.6) | 1.2 (0.9–1.5) | 1.1 (0.9–1.3) |
| 10,000 and above | 31 (32.6) | 64 (67.4) | Ref | |
| Breast self-examination | ||||
| Not done | 26 (23.6) | 84 (76.4) | 2.4 (1.2–5.1) | 1.8 (0.8–3.8) |
| Done | 11 (68.3) | 5 (31.3) | Ref | |
| Breast cancer information | ||||
| Not received | 30 (25.9) | 86 (74.1) | 2.5 (0.9–6.4) | 1.9 (0.8–4.6) |
| Received | 7 (70) | 3 (30) | Ref |
The adjusted prevalence ratio was calculated using log-binomial regression. Variables found significant in univariate analysis at P<0.2 were included. CI: Confidence interval, Ref: Reference category
Reasons for delay
Patient delay
The causes for patient delay are summarised in Table 4.
| Reasons for delay | Percentage among patients presenting ≥3 months (%) |
|---|---|
| Considered as harmless | 83.1 |
| Considered as temporary | 80.9 |
| Age-related change | 14.6 |
| Considered as benign | 74.2 |
| Considered as infection | 1.1 |
| Considered a small size to be cancer | 33.7 |
| Time constraints | 2.2 |
| Fear of diagnostics | 24.7 |
| Reluctant to show breast complaints | 44.9 |
| Painless | 68.5 |
| Took alternate treatment initially | 2.2 |
JIPMER: Jawaharlal Institute of Postgraduate Medical Education and Research
Provider delay
In our study, the average time taken by the patients to present to JIPMER for definitive management of breast cancer after visiting a local physician was a median of 25 days and a mean of 48.77 days, ranging from 2 days to 1 year.
System delay
In our study, the time taken for confirmation of diagnosis from the time of presentation to JIPMER was a median of 13 days and a mean of 16.58 days, with a standard deviation of 12.31 ranging from a minimum of 2 days to a maximum of 83 days. About 90% of the patients had their diagnosis confirmed within 1 month.
DISCUSSION
India has a lower incidence of breast cancer as compared to the West. The age at presentation is also younger in India. Despite the low incidence and younger patients, the mortality rate is higher than in the West.[1,3,14] This is due to the delays at all levels of healthcare. Most studies in India and other developing countries attribute much of the delay to patient delay.[11,15,16] Countries like Mexico, which have implemented population education and have a screening mammogram program, have successfully reduced patient delay and are finding ways to reduce provider delay.[17] Developed countries are in the process of tackling system delays.[18] The patient delay can be overcome only after understanding the causes of the delay as these causes are highly dependent on the sociodemographic makeup of the population, the causes, and, hence, the methods to overcome them will need to be tailored to the population.
It has been shown that a delay of 3 months leads to significant deterioration in the prognosis of patients with breast cancer.[2] Studies done in India all show that most patients present later than 3 months. These studies were retrospective or from cancer databases. Most of these studies in the past are also aware of the differences between the population in different regions of India and make a distinction between South, North, Northeast and Central India where these studies were conducted.[11,15,19-21] Ours was a prospective study conducted at a large tertiary care centre in South India. It aims to understand the factors and causes of patient delay so that appropriate measures can be taken to overcome them.
In our study, out of 126 patients, 37 patients (29.4%) presented early, and the rest, 89 patients (70.6%), presented later than 3 months. This is similar to a past study conducted in Delhi, where 61.6% presented later than 3 months.[22] In contrast, 17.4% of patients presented late in a study done in Germany[8] and 20.3% presented late in a study in Columbia.[23] Patients present earlier in the high-income and developed countries compared to developing and low-income countries.
The median patient interval between symptom recognition and presentation in high-income countries is 7–16 days.[24] In our study, the median interval was found to be 4 months. This reflects the differences in the level of awareness of breast cancer symptoms and the interpretation of symptoms by the patients in the developed and developing countries, which was also demonstrated by past studies. This emphasises the importance of population awareness regarding breast cancer, an area which needs improvement in the Indian population.
Other factors which highlight the importance of population awareness are the differences between the rural and urban populations. In our study, patients from rural areas presented late compared to those from urban areas. Among patients from rural areas, 84.6% presented late compared to 60.8% from urban areas. The educational status of the patient was found to have an impact on the presentation delay of the patients. In our study, as the educational level of the patient increased, they tended to present earlier. This shows a lack of knowledge regarding breast cancer symptoms and health awareness among patients with low educational status.
The delay in presentation also leads to the presentation of patients with advanced disease, as opposed to developed countries, where patients present at earlier stages. In our study, among the patients presenting without delay, the majority were in stage 2, whereas among the patients with delay, the majority were in stage 3. Thus, a delay in presentation leads to the disease being diagnosed at an advanced stage.
There was no significant association found between income and occupation of the patient, presence or absence of comorbid illness, menopausal status and parity on patient delay in our study. The association between marital status, family history and history of benign breast diseases on delay could not be commented on due to their small numbers in our study.
Similar to past studies in our study, too, patients who practised breast self-examination tended to present earlier to healthcare providers.[25,26] According to some studies, women who regularly practised breast self-examination presented with smaller tumours and were less likely to have nodal involvement.[27-30] However, some studies show no benefit with breast self-examination. Breast self-examination was not recommended as a screening method by the World Health Organization. Still, some healthcare providers encourage breast self-examination as a quality healthcare practice to detect palpable breast lumps.[31]
In our study, 10 patients (7.9%) were provided information regarding breast cancer prior to their lives from a reliable source, which included healthcare professionals or mass media. Among those who were aware of the breast cancer symptoms, 70% presented early. This exemplifies the importance of health education in promoting patient awareness and health-seeking behaviour.
In our study, out of 126 patients, 125 had painless breast lumps as their first symptom. Only one patient has breast pain as her first symptom. However, most of them waited until they developed other symptoms such as pain (36.5%), nipple discharge (4%), nipple distortion (3.2%), ulceration (7.1%), axillary swelling (3.2%) or supraclavicular swelling (0.8%) before presenting to a health-care provider. Patients, presentation to a health-care provider depends on the interpretation of their symptoms as a serious health issue.[32] This is a common theme among patients in India where the patients tend to present when the symptoms turn distressing or hamper activity.
Among the patients who presented late, the majority of them (83.1%) felt that the symptoms were harmless. Most of them thought that the symptoms were temporary (80.9%). About 74.2% thought that it could be a benign disease. This misinterpretation of the symptoms is due to a lack of awareness regarding breast cancer and its symptoms. This problem is especially high in painless malignancies like breast cancer, as the patients tend to ignore the lump as it is painless.
Out of 126 patients, 43 patients (34.1%) said that they were reluctant to visit a healthcare provider for breast complaints due to shyness or shame. According to a study in North Pakistan, 10.6% of the patients delayed presentation as they were reluctant to visit male doctors for breast complaints.[16] This reluctance to visit healthcare facilities for breast complaints is due to cultural factors in developing countries, which can be overcome by proper health education.
In our study, 3 patients (0.2%) received traditional medication initially for the lump and then presented to the qualified healthcare provider as the lump had not decreased in size. This number is significantly lesser than the past studies in India and other countries but it remains a challenge which needs to be overcome.[19,33]
Our study was based on a detailed questionnaire that inspected all potential causes of patient delay. The patients were interviewed, and provisions were made to incorporate their views and reasons for the delay instead of adhering to only a strict questionnaire.
As this was based on patient recall, there can be some recall bias. This was overcome by giving the patients who were not sure if the symptoms were for 3 months or longer a benefit of the doubt and including them in a delay group. The other drawback of this study is the sample size, which was small for studying the factors associated with delay. This may be a reason for not finding any significant predictor in multivariate analysis. Future studies with larger sample sizes will help in identifying factors associated with delay.
CONCLUSION
In our study, the proportion of delayed presentation among breast cancer patients was found to be 70.6%. Patients from rural areas and with lower educational status were found to have a higher incidence of delayed presentation. Lack of awareness of breast cancer symptoms and their misinterpretation as harmless, temporary and benign are the main reasons for delayed presentation. Breast cancer awareness programmes should be designed to create breast cancer awareness among people, particularly targeting the rural population and those with lower educational status. Patients who practised breast self-examination presented earlier. Breast self-examination and clinical breast examination can be encouraged as screening tools for diagnosing breast cancer in the early stage. Models can be adapted for spreading awareness, health-seeking behaviour and population screening from developed countries that have overcome these hurdles in the past. Further studies with a larger sample will help in identifying the other sociodemographic and clinical characteristics responsible for delayed presentation.
Ethical approval
The study was approved by JIPMER’s postgraduate research monitoring committee and the Institute Human Ethics Committee (IEC) number (ECR/342/Inst/PY/2015/RR-13) dated 5-12-2015.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Funding for the trial was obtained from the Institutional Intramural Research Fund Committee, JIPMER.
References
- GLOBOCAN 2020 Report on Global Cancer Burden: Challenges and Opportunities for Surgical Oncologists. Ann Surg Oncol. 2022;29:6497-500.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Predicting Delayed Presentation of Symptomatic Breast Cancer: A Systematic Review. Lancet. 1999;353:1127-31.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed Presentation and Diagnosis of Breast Cancer in African Women: A Systematic Review. Ann Epidemiol. 2017;27:659-71.e7.
- [CrossRef] [PubMed] [Google Scholar]
- Potential Risk Factors Influencing the Formation of Postoperative Seroma After Breast Surgery-A Prospective Study. Anticancer Res. 2021;41:859-67.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic Patient Characteristics Predict Delay in Cancer Diagnosis: A Danish Cohort Study. BMC Health Serv Res. 2008;8:49.
- [CrossRef] [PubMed] [Google Scholar]
- The Andersen Model of Total Patient Delay: A Systematic Review of its Application in Cancer Diagnosis. J Health Serv Res Policy. 2012;17:110-8.
- [CrossRef] [PubMed] [Google Scholar]
- Delay in Seeking a Cancer Diagnosis: Delay Stages and Psychophysiological Comparison Processes. Br J Soc Psychol. 1995;34:33-52.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Delay and Stage of Diagnosis among Breast Cancer Patients in Germany--a Population Based Study. Br J Cancer. 2002;86:1034-40.
- [CrossRef] [PubMed] [Google Scholar]
- Influences on Pre-Hospital Delay in the Diagnosis of Colorectal Cancer: A Systematic Review. Br J Cancer. 2008;98:60-70.
- [CrossRef] [PubMed] [Google Scholar]
- A Systematic Review of Barriers to Breast Cancer Care in Developing Countries Resulting in Delayed Patient Presentation. J Oncol. 2012;2012:121873.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Socio-Economic and Demographic Factors in Delayed Reporting and Late-Stage Presentation among Patients with Breast Cancer in a Major Cancer Hospital in South India. Asian Pac J Cancer Prev. 2008;9:703-7.
- [Google Scholar]
- Delayed Presentation in Breast Cancer: A Study in Iranian Women. BMC Womens Health. 2003;3:4.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Delay in Women Presenting with Advanced Breast Cancer: An Iranian Study. Public Health. 2005;119:885-91.
- [CrossRef] [PubMed] [Google Scholar]
- Delays in Breast Cancer Detection and Treatment in Developing Countries. Breast Cancer (Auckl). 2018;12:1178223417752677.
- [CrossRef] [PubMed] [Google Scholar]
- Delay in Presentation to the Hospital and Factors Affecting it in Breast Cancer Patients Attending Tertiary Care Center in Central India. Indian J Cancer. 2015;52:102-5.
- [CrossRef] [PubMed] [Google Scholar]
- Presentation Delay in Breast Cancer Patients, Identifying the Barriers in North Pakistan. Asian Pac J Cancer Prev. 2015;16:377-80.
- [CrossRef] [PubMed] [Google Scholar]
- Non-Timely Referral of Women Aged 40 to 69 to Preventive Medicine for Breast Cancer Detection and its Association with the BI-RADS Classification. Prev Med Rep. 2023;35:102369.
- [CrossRef] [PubMed] [Google Scholar]
- Timing and Delays in Breast Cancer Evaluation and Treatment. Ann Surg Oncol. 2018;25:2829-38.
- [CrossRef] [PubMed] [Google Scholar]
- Delays in Diagnosis and Treatment of Breast Cancer and the Pathways of Care: A Mixed Methods Study from a Tertiary Cancer Centre in North East India. Asian Pac J Cancer Prev. 2019;20:3711-21.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Features and Prognostic Factors of Early Breast Cancer at a Major Cancer Center in North India. Indian J Cancer. 2005;42:40-5.
- [CrossRef] [PubMed] [Google Scholar]
- Presentation Delay in Breast Cancer Patients and its Association with Sociodemographic Factors in North Pakistan. Chin J Cancer Res. 2015;27:288-93.
- [Google Scholar]
- Stage at Diagnosis and Delay in Seeking Medical Care among Women with Breast Cancer, Delhi, India. Iran Red Crescent Med J. 2014;16:e14490.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Delay among Colombian Women with Breast Cancer. Salud Pública Méx. 2009;51:372-80.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges to the Early Diagnosis and Treatment of Breast Cancer in Developing Countries. World J Clin Oncol. 2014;5:465-77.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of Breast Self-Examination for an Early Detection of Breast Cancer Results of a Study on 500 Breast Cancer Patients and 652 Controls. Tumori. 1981;67:219-24.
- [CrossRef] [PubMed] [Google Scholar]
- Behavioral and Biological Determinants of Surgical Stage of Breast Cancer. Prev Med. 1982;11:429-40.
- [CrossRef] [PubMed] [Google Scholar]
- Breast Self-Examination and Medical Examination Related to Breast Cancer Stage. Am J Public Health. 1981;71:583-90.
- [CrossRef] [PubMed] [Google Scholar]
- Breast Self-Examination, Relationship to Stage of Breast Cancer at Diagnosis. Cancer. 1981;47:2740-5.
- [CrossRef] [PubMed] [Google Scholar]
- Breast Self-Examination Practices and Breast-Cancer Stage. N Engl J Med. 1978;299:265-70.
- [CrossRef] [PubMed] [Google Scholar]
- Breast Self Examination and Breast Cancer Stage at Diagnosis. Br J Cancer. 1987;55:207-11.
- [CrossRef] [PubMed] [Google Scholar]
- Can Breast Self-Examination Continue to be Touted Justifiably as an Optional Practice? Int J Surg Oncol. 2011;2011:965464.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of Breast Cancer Across the Lifespan. J Psychosom Res. 2003;54:141-6.
- [CrossRef] [PubMed] [Google Scholar]
- Complementary and Alternative Medicine (CAM) Use and Delays in Presentation and Diagnosis of Breast Cancer Patients in Public Hospitals in Malaysia. PLoS One. 2017;12:e0176394.
- [CrossRef] [PubMed] [Google Scholar]