Translate this page into:
Impact of Psychological and Socioeconomic Factors on Management of Bone Tumours with Custom-made Endoprosthesis Reconstruction

*Corresponding author: Subbiah Shanmugam, Department of Surgical Oncology, Government Royapettah Hospital, Chennai, Tamil Nadu, India. subbiahshanmugam67@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shanmugam S, Balakrishnan S. Impact of Psychological and Socioeconomic Factors on Management of Bone Tumours with Custom-made Endoprosthesis Reconstruction. Indian Cancer Awareness J. 2024;3:55-8. doi: 10.25259/ICAJ_27_2023
Abstract
Objectives:
In the past few decades, the definitive treatment for bone tumours has evolved considerably. Resection followed by custom-made endoprosthesis reconstruction has become the standard of care. The main objective of this study is to analyse the psychological and socioeconomic factors impacting the treatment of bone tumours.
Materials and Methods:
Among the 53 patients who underwent bone resection with custom mega prosthesis (CMP) reconstruction between 2013 and 2022, 22 patients are in regular follow-up, 16 patients are lost in follow-up, and the remaining 15 are dead. We prepared a questionnaire which included 22 questions to assess the impact of psycho-social and economic factors on the treatment of bone tumours.
Results:
We included 22 patients in our study. The average total duration of disease before surgery was 95 days. The average days of in-hospital stay was 53 days. The average number of days of hospital stay after surgery was 14 days. The average amount spent during the hospital stay was about 240 Indian national rupees/day. The average loss of work was about 90 days. The average days of leave availed in school/college was 135 days. About 69.2% of patients had to go for a change of occupation. About 90.9% of patients had a fear of recurrence. About 77.2% of patients found it difficult to indulge themselves in recreational/sports activities. About 45.4% of patients felt it was difficult for their partner/family to empathise with their situation. About 59% of patients had sleep difficulties. About 36.3% of patients were well satisfied with their prosthesis.
Conclusion:
Being predominantly a disease of the young population, the need for comprehensive management, including psychological counselling and rehabilitation in addition to cancer treatment, seems to be the need of the hour. The fact of the high cost of non-treatment-related expenditure needs to be addressed. A frequent cancer survivor programme will aid these patients to regain their self-confidence.
Keywords
Bone tumors
Custom-made mega prosthesis
Economic
Psychological
INTRODUCTION
Treatment options for bone tumours have changed significantly during the past few decades. A combination of chemotherapy, radiation therapy and surgery is used in the multidisciplinary treatment.[1] Previously, amputation was considered the principal surgical treatment assuring a radical margin; however, improved chemotherapy schedules permit sparing the limb and increased survival.[2,3]
Most of our patients belong to lower and upper socioeconomic classes.[4] The word ‘cancer’ creates immense psychological stress, not only for the patient but also for their families, and a proper psychological support system may improve this scenario.
Aim and objective
To analyse the socioeconomic factors of the patients who underwent bone tumour resection with reconstruction and its impact on the quality of life (QOL) of patients and their families after treatment of the disease
To determine the psychological impact on patients and to analyse the necessity of early psychological intervention.
MATERIALS AND METHODS
We analysed the patients who underwent bone resection with custom-made prosthesis reconstruction in our institution between 2013 and 2022. We included all patients from 10 years to 60 years of age. We excluded the patients who are not in follow-up and patients who have expired. We prepared a questionnaire which included 22 questions to assess the impact of psycho-social and economic factors on the treatment of bone tumours.
Questionnaire
Name:
Age/sex:
Occupation:
Father’s/spouse occupation:
Income:
Marital status:
Total duration of disease before surgery:
Total number of days of hospital stay:
-
Number of chemotherapies administered
Pre-operative
Post-operative.
Number of days of hospital stay after surgery:
-
Any readmission after surgery (excluding for the purpose of chemotherapy)
If Yes, then the reason:
Average amount spent (Indian national rupees- INR/day) during the hospital stay
Average amount spent in total:
Average days of loss of work:
Average days of leave availed to school/college:
-
Any change of occupation: Yes/No
If Yes, then reason:
I’m afraid that my disease will recur: Yes/No
It’s difficult to take part in recreational/sport activities: Yes/No
It’s difficult for my partner/family to empathise with my situation: Yes/No
I have difficulties in sexual life after treatment: Yes/No
I have difficulties in sleep at night: Yes/No
-
Overall satisfaction after prosthesis reconstruction: Yes/No.
If No, then reason:
We obtained data from the questions either from patients or from their parents if the patient is under 18. The questionnaire is based on modifications of the EORTC core QOL questionnaire-C30, Toronto extremity salvage score, and musculoskeletal tumour society questionnaire.
RESULTS
The average monthly income for the patient/head of family is 16500 INR (4500–33000 INR).
The average duration from diagnosis to the start of treatment was 26 days. (19–33 days). The average total duration of disease before surgery was 95 days (which includes chemotherapy and a plan for prosthesis). The average days of in-hospital stay was 53 days. The average number of days of hospital stay after surgery was 14 days (10–18 days).
The average amount spent during the hospital stay was about 240 INR/day (in spite of providing food to patients free of cost), or around 12720 INR. The average amount spent on transport alone was 84000 INR.
The average loss of work after surgery was about 90 days (60–120 days). The average days of leave taken in school/college were 135 days. Hence, in total, there was a loss of work for a period of around seven and a half months. About 92.3% of these patients were not paid any kind of salary/compensatory pay during these days.
About 69.2% of patients had to change occupations, and 55.5% were forced to quit their occupations. About 90.9% of patients had a fear of recurrence. About 77.2% of patients found difficulty indulging in recreational/sports activities. This figure reaches up to 94.1% if the tumour involves the lower extremities.
About 45.4% of patients felt that their family members were unable to empathise with their situation. About 59% of patients had sleep difficulties. About 72.7% had difficulties in sexual life after treatment.
About 36.3% of patients were well satisfied with their prosthesis. About 31.85% were satisfied but not up to their expectations, while 31.85% were not satisfied with the prosthesis.
DISCUSSION
According to the modified Kuppuswamy classification[4] for socioeconomic status, which is widely used in our country, most of our patients belong to the lower and upper classes. As per this classification, the average income for lower socioeconomic status is <9307 INR. In our study, the average per capita income is 16500 INR.
Most of our patients were not able to get the appropriate initial form of treatment, such as a proper biopsy or initiation of chemotherapy, for a period of one month. During this one-month duration, some of our patients may even end up undergoing inappropriate investigation or inappropriately placed biopsy. This adds up to an additional economic burden and may impact the performance of the limb salvage surgery.
The daily average amount spent during the hospital stay was about 240 INR, and the major portion of this goes to meet the need for food for the attenders [Graph 1]. The average number of attendees per person was two. So, for daily expenses alone, they have to spend around three-fourths of their average monthly income during their hospital stay. These expenses can be cut short to some extent if we restrict the number of attendees to the patient to one during the hospital stay.
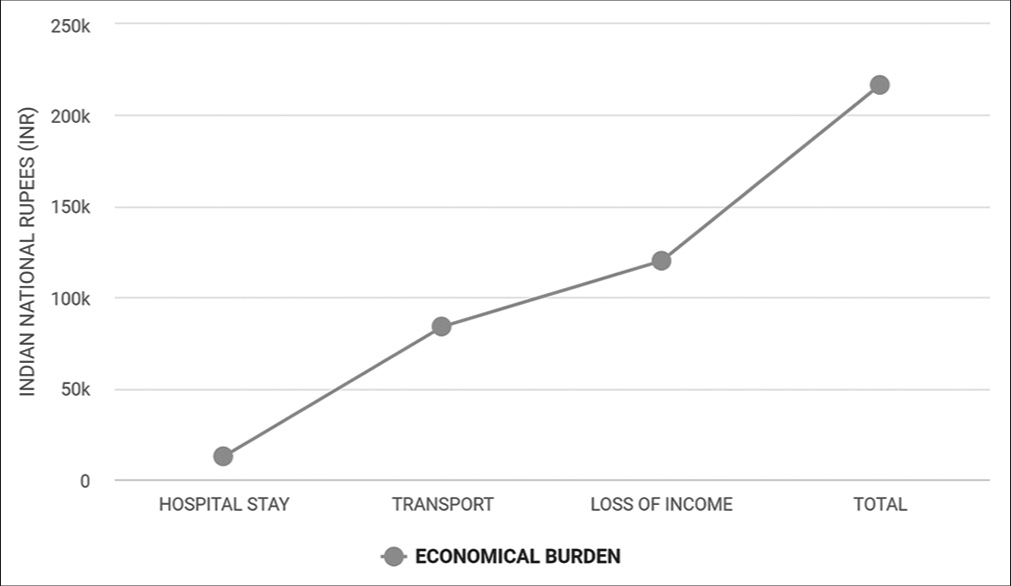
- Economic burden.
One of the huge expenditures during the treatment course was transportation. The average cost for transportation during the treatment course was about 84,000 INR [Graph 1]. Since public transport is not compatible with musculoskeletal tumour patients, most of our patients prefer private transportation to reach the hospital from different parts of our state.
The average period of loss of work was about 7½ months (which includes both treatment course and post-operative and rehabilitation period) in 1 year. So for these 7½ months, 92.3% of patients were not paid any salary or compensation, and it almost led to a loss of about 1.2 lakhs INR. Hence, in total, the average economic deficit crosses more than 2 lakhs INR, which surpasses the average 1-year income of the patient [Graph 2].
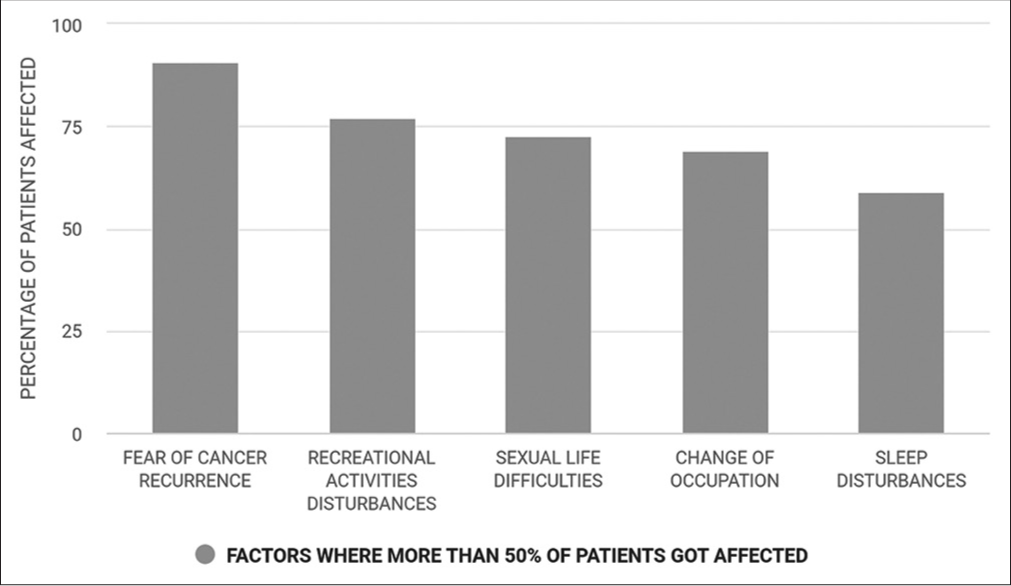
- Factors where more than 50% of patients were affected.
Among these patients, 69.2% had to go for a change of occupation [Graph 2]. The irony is some of the patients were forced to quit their jobs by their employers due to the fear of cancer spreading to them [Graph 2]. This reflects badly on awareness about cancer and its spread among the general public in developing countries.
Cancer patients often endure pain, which can significantly increase their anxiety, despair and sense of helplessness.[5-7] Patients may have pain as a direct result of their underlying illness or as a result of treatments such as radiation therapy, chemotherapy or surgery used to treat their cancer. This leads to sleep disturbances and a lack of interest in sexual activities in our patients [Graph 2]. This can be encountered by proper psychological counselling and with adequate and prompt physiotherapy along with proper analgesics.
The majority of cancer patients experience varied degrees of psychological stress, one of which is fear of cancer recurrence (FCR).[8] In our study, almost more than 90% of patients experience the FCR. Numerous research has discovered a link between high FCR and poor QOL, psychological comorbidities, increased distress and physical limits.[9-11]
Participating in sports and other physical and recreational activities has never been easy for cancer survivors. Recreational activity restriction in our patients is largely influenced by psychological despair and pain, in addition to the moderate physiological restrictions following a custom-made endoprosthesis reconstruction. Yet, research has shown that exercise helps cancer survivors in several ways, including psychological and QOL outcomes, physical functioning, body weight and composition, immune system performance and cardiovascular fitness.[12]
Summarising all the above factors, the overall satisfaction for the custom-made endoprosthesis in bone tumours is about 36.3% only [Graph 3]. The remaining patients are either not at all satisfied or have very high expectations about the custom-made endoprosthesis and its function.
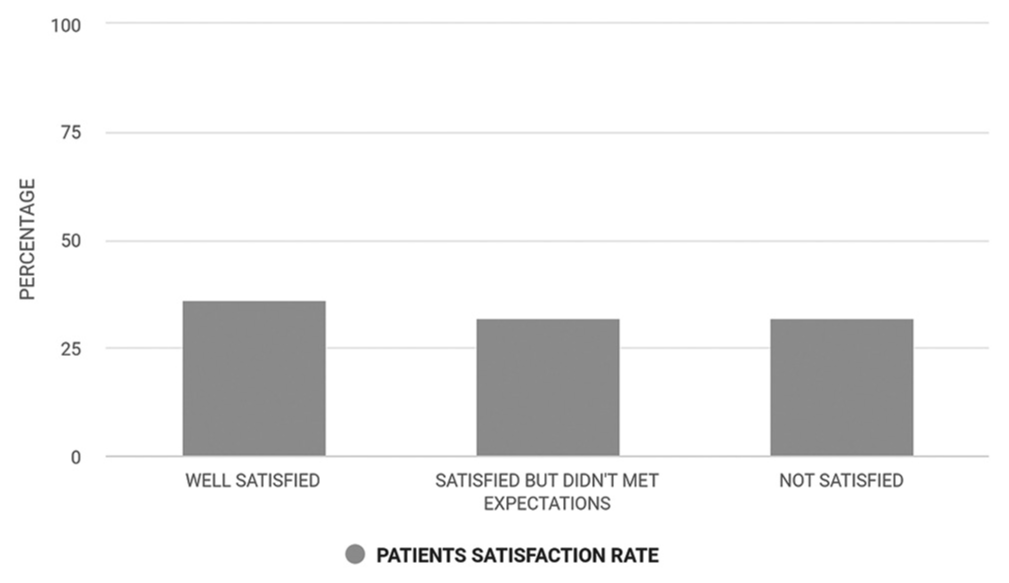
- Patients’ satisfaction rate.
Challenges ahead
The existing healthcare delivery system cares more about treatment and less about psychological and occupational rehabilitation. Proper psychological counselling and rehabilitation in both the preoperative and postoperative periods may help to improve the overall outcome.
Prompt early physiotherapy and professional reintegration help them to lead a good QOL in society. We must educate the general population about cancer to knock off the myths and rumours revolving around cancer.
CONCLUSION
There should be direct coordination between health care providers – social welfare department – policy makers. To reduce the financial burden and to improve QOL, services like the national cancer helpline along with a cancer care ambulance for transportation might help the patients, especially for musculoskeletal cancer. Frequent cancer survivor programmes will aid these patients to regain their self-confidence.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Current Review of Surgical Management Options for Extremity Bone Sarcomas. EFORT Open Rev. 2019;4:174-82.
- [CrossRef] [Google Scholar]
- Current Status of Management and Outcome for Patients with Ewing Sarcoma. Cancers (Basel). 2021;13:1202.
- [CrossRef] [Google Scholar]
- Adjuvant and Neoadjuvant Combination Chemotherapy for Osteogenic Sarcoma. Curr Opin Oncol. 2007;19:341-6.
- [CrossRef] [Google Scholar]
- Modified Kuppuswamy Socioeconomic Scale: 2022 Update of India. Int J Community Med Public Health. 2022;9:3841.
- [CrossRef] [Google Scholar]
- Examining the Influence of Coping with Pain on Depression, Anxiety, and Fatigue among Women with Breast Cancer. J Psychosoc Oncol. 2005;23:137-57.
- [CrossRef] [Google Scholar]
- The Cancer Patient with Pain: Psychiatric Complications and their Management. Med Clin North Am. 1987;71:243-58.
- [CrossRef] [Google Scholar]
- Fear of Cancer Recurrence: A Practical Guide for Clinicians. Oncology (Williston Park). 2018;32:32-8.
- [Google Scholar]
- Fear of Recurrence among Older Breast, Ovarian, Endometrial, and Colorectal Cancer Survivors: Findings from the WHI LILAC Study. Psychooncology. 2018;27:1810-5.
- [CrossRef] [Google Scholar]
- Health Anxiety and Illness-Related Fears Across Diverse Chronic Illnesses: A Systematic Review on Conceptualization, Measurement, Prevalence, Course, and Correlates. PLoS One. 2020;15:e0234124.
- [CrossRef] [Google Scholar]
- Fear of Cancer Recurrence in Adult Cancer Survivors: A Systematic Review of Quantitative Studies. J Cancer Surviv. 2013;7:300-22.
- [CrossRef] [Google Scholar]







