Translate this page into:
Incidental Hypercalcemia: The Sole Presentation of B-Cell Acute Lymphoblastic Leukaemia

*Corresponding author: Poonam Gupta, Professor and Head, Department of Medicine, Moti Lal Nehru Medical College, Prayagraj, Uttar Pradesh, India. poonam_gupta16@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta P, Chaurasia AK, Guatam AK. Incidental Hypercalcemia: The Sole Presentation of B-cell Acute Lymphoblastic Leukaemia. Indian Cancer Awareness J. 2024;3:62-5. doi: 10.25259/ICAJ_5_2024
Abstract
This article aims to report a sole presentation of B-cell acute lymphoblastic leukaemia (ALL) as incidental hypercalcemia. ALL is the most frequent neoplastic disease in children, with an early peak at the age of 3–4 years. ALL presents with neutropenic fever, bruising, anaemia, lymphadenopathy and bone pain. Presenting features as manifestations of hypercalcemia in ALL is extremely rare, especially in adults. More than 90% of causes of hypercalcemia are primary hyperparathyroidism and malignancy. Hence, if parathyroid hormone (PTH) levels come low, malignancy is the most probable aetiology. Hypercalcemia associated with malignancy includes three distinct syndromes. Bone metastases may cause hypercalcemia. Direct bone marrow invasion occurs with hematologic malignancies such as leukaemia, lymphoma and multiple myeloma. Hypercalcemia is seen in <1% of cases of leukaemia. A 16-year-old male presented with nausea, vomiting, abdominal pain and burning micturition. Physical examination was unremarkable except for pallor. His laboratory studies showed haemoglobin 5.7g/dL, white cell count 5700/mm3, platelet count 51,000/dL, and serum calcium 17.1 mg/d. He was hydrated and given zoledronate IV, with which calcium level normalised and symptoms resolved. The patient had low PTH and low parathyroid hormone-related peptide (PTHrp). Peripheral smear and bone marrow showed lymphoblasts. Flow cytometry confirmed B-cell ALL with 43% blasts. Hypercalcemia revealed B-cell ALL in an adult after a thorough workup of low PTH and PTHrp, peripheral blood picture, bone marrow examination, and flow cytometry. Hence, ALL should be considered in the differential diagnosis of a young adult presenting with incidental hypercalcemia.
Keywords
Hypercalcemia
Low parathyroid hormone
Low parathyroid hormone-related peptide
B-cell acute lymphoblastic leukaemia
INTRODUCTION
Acute lymphoblastic leukaemia (ALL) is the most frequent neoplastic disease in children, with an early peak at the age of 3–4 years. The incidence in adults ranges from 0.7 to 1.8/100 000/year, being somewhat higher in adolescents and young adults. The aetiology of acute leukaemias is unknown. Internal and external factors influence the incidence of leukaemia. ALL presents with neutropenic fever, bruising, anaemia, lymphadenopathy and bone pain. The diagnosis of acute leukaemia is first made by examination of the peripheral blood and bone marrow. For further classification of the leukemic blast cells, cytochemical stains, immunologic markers and cytogenetic and molecular analysis are required. The immunologic markers are still the major criteria to subdivide into B-cell lineage or T-cell lineage ALL leukemias.[1]
More than 90% of causes of hypercalcemia are primary hyperparathyroidism and malignancy. So if parathyroid hormone (PTH) levels come low, malignancy is the most probable aetiology.[2] Hypercalcemia is a rare event in most haematological malignancies except in patients with multiple myeloma and in adult T-cell leukaemia (ATLL)/lymphoma, in whom it is commonly seen. Incidence of hypercalcemia varies from 50% to 90% in ATLL, 27–35% in lung cancers, 25–30% in breast cancer, 7–30% in multiple myeloma but <10% in lymphomas and even <1% in leukaemias.[2] While mild hypercalcemia may be asymptomatic, moderate-to-severe hypercalcemia can be associated with a variety of symptoms. There are more cases reported of B-cell ALL-associated hypercalcemia in children, but only a few have been found in young adults.[3]
CASE REPORT
About 16-year-old male presented with nausea and three episodes of vomiting for 3 weeks, pain abdomen for 2 weeks and burning micturition for 2 weeks in SRN Hospital of Moti Lal Nehru Medical College, Prayagraj Uttar Pradesh, India.
Clinical examination
Physical examination on admission showed lethargy and apathy. His pulse rate was 126/min, axillary temperature 37.2°C, blood pressure 112/78 mmHg, weight 45 kg and respiratory rate 20/min. His skin and oral mucosa were dry due to dehydration. No hepatomegaly, splenomegaly or lymphadenopathy was detected. The rest of his physical examination findings were unremarkable.
Investigations and treatment
The patient was approached and investigated properly as shown in Table 1. As the patient came out to be of hypercalcemia, so hypercalcemia was treated with intravenous isotonic sodium chloride solution, furosemide and Zolendronic acid. The patient also had creatinine 2.2 mg/dL; after 24 h of treatment, serum calcium and creatinine decreased to the normal level. Urine showed Klebsiella, and levofloxacin was given. Serum PTH and parathyroid hormone-related peptide (PTHrp) were done to evaluate the cause of hypercalcemia according to the flow chart described in Figure 1.
| Hb | 5.7 g/dL | 11.5–15.5 g/dL |
| TLC | 3800 cell/mm3 | 4000–11000 cells/mm3 |
| Platelet | 0.51 lac cell/mm3 | 1.5–4.0 lac cells/mm3 |
| Serum urea | 40 mg/dL | 13–43 mg/dL |
| Serum creatinine | 2.2 mg/dL | 0.6–1.2 mg/dL |
| Reticulocyte count | 1.9% | 0.5–2.5% |
| Urine routine and microscopy | 8–12 PUS Cells | 0–4 pus cells |
| Urine culture | Klebsiella | |
| Serum calcium | 17.1 mg/dL | 8.6–10.2 mg/dL |
| Serum albumin | 3.8 mg/dL | 3.2–4.6mg/dL |
| Serum intact PTH | 2.1 pg/dL | 15–65pg/mL |
| Vitamin D 25 hydroxy | 11.2 ng/mL | 20–50 ng/mL |
| Vitamin D 1,25 Dihydroxy | 5 pg/mL | 19.6–54.3 pg/mL |
| Serum PTHrp | 2 pmol/L | Less than 2.5 pmol/L |
| USG whole abdomen with KUB | Bilateral normal-sized kidney and MRD grade 1 | |
| ECG | OTc(corrected QT) interval shortening (320 ms) | |
| Chest X-ray and X-ray of skull and spine | Showed no osteolytic lesions | |
| CT chest and abdomen | Showed no evidence of malignancy |
PTH: Parathyroid hormone, PTHrp: Parathyroid hormone-related peptide, TLC: Total leucocyte count, Hb: Haemoglobin, CT: Computed tomography, ECG: Electrocardiogram, USG: Ultrasound, KUB: Kidney, ureter and bladder, MRD: Medical renal disease, QTc: corrected QT interval
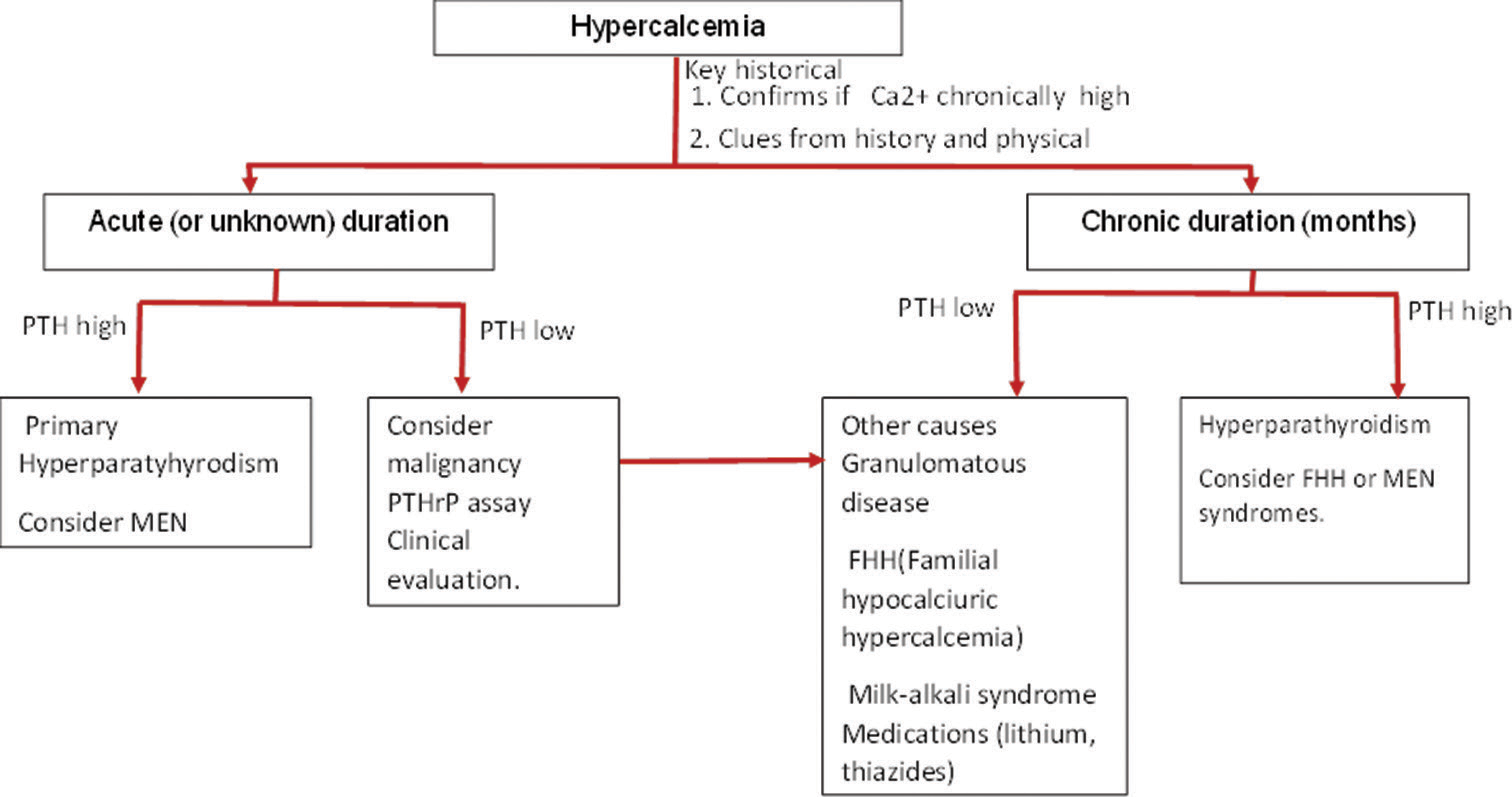
- Flow chart showing the approach to patient hypercalcemia. PTH: Parathyroid hormone, PTHrP: Parathyroid hormone related peptide, MEN: Multiple endocrine neoplasia
As the PTH and PTHrp were low, a peripheral smear was done to further evaluate in search of malignancy, which showed lymphoblasts. The peripheral smear showed blast cells with a high nuclear-cytoplasmic ratio, coarse nuclear chromatin, and scanty cytoplasm suggestive of acute leukaemia. Bone marrow aspiration showed 80% lymphoblasts [Figure 2].
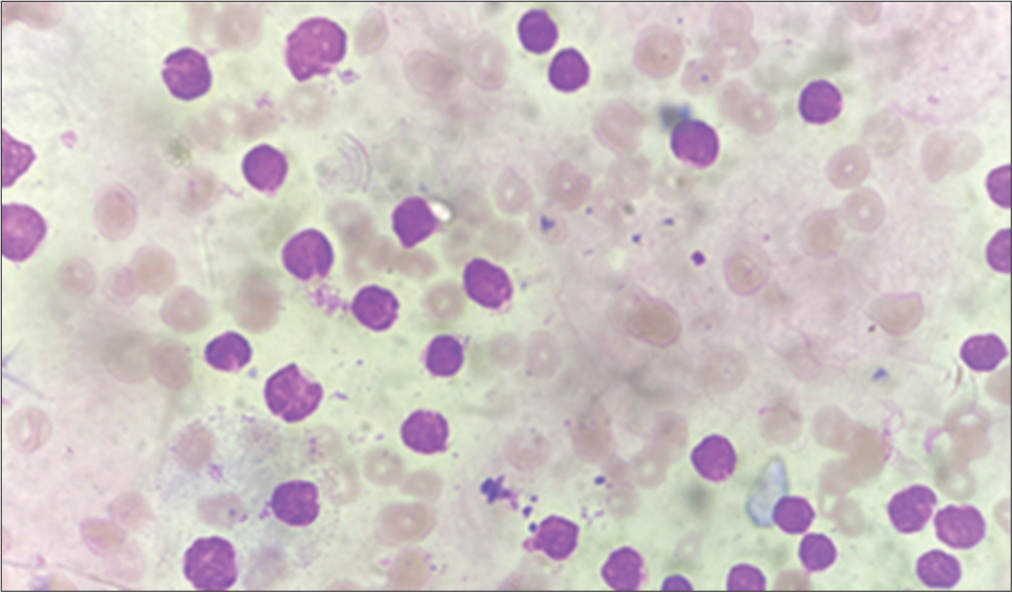
- Acute lymphoblastic leukaemia (×100): The patient’s peripheral blood smear shows the presence of blast cells, which are small and uniform in size with scanty cytoplasm. Nuclei have coarsely clumped chromatin and indistinct nucleoli.
After that, flow cytometry was done, and it showed 75% blast cells expressing moderate CD10, CD19, CD20, CD38 and CD22 markers suggestive of B-cell lineage of ALL. Blast cells were negative for T-cells and myeloid lineage. Chest X-ray and X-ray skull and spine showed no osteolytic lesions. Computed tomography chest and abdomen showed no evidence of malignancy. A lumbar puncture for cerebrospinal fluid analysis was also done to rule out central nervous system leukaemia, and it came out to be normal. Thus, after cytogenetic and flow cytometric analysis, the patient was diagnosed with ALL of the B-cell types.
DISCUSSION
Hypercalcemia has been described in children with hematologic malignancies and solid tumours. It is extremely rare to see it in adults with leukaemia.[3] Gastrointestinal (nausea, vomiting, anorexia and constipation), neuromuscular (lethargy, fatigue, hypotonia, stupor and coma), and cardiovascular (bradycardia and arrhythmia) symptoms characterise the clinical spectrum of malignant hypercalcemia.[4] The white blood cell count in 40% of ALL patients is reduced or normal. In 8% of ALL patients, no circulating leukemic blast cells are seen. Thus, in the frequently used automatic blood cell counting, the diagnostic features may not be seen.[1] Primary hyperparathyroidism and malignancy account for >90% of all cells of hypercalcemia. Hypercalcemia associated with malignancy includes three distinct syndromes.[5]
Bone metastasis
Humoral hypercalcemia of malignancy PTH: Parathyroid Hormone, PTHrP: Parathyroid Hormone Related peptide, MEN: Multiple Endocrine Neoplasia
Direct bone marrow invasion occurs with haematological malignancies such as leukaemia, lymphoma and multiple myeloma.
Humoral hypercalcemia of malignancy is mediated primarily by PTHrp) which is responsible for paraneoplastic hypercalcemia. Direct bone marrow invasion occurs by malignancies such as leukaemia, lymphoma and multiple myeloma. Lymphokines and cytokines such as interleukin-1, lymphotoxin and tumour necrosis factor-alpha produced by cells involved in bone marrow invasion promote resorption of bone through local destruction, thus producing hypercalcemia and suppressing the parathyroid gland that makes the PTH levels low or undetectable.[1] PTHrP produced by lymphoblasts causes hypercalcemia, but Rizolli et al.[6] reported a lower prevalence of elevated PTHrP in hematopoietic malignancies. (21%) as compared to other malignancies as lung & Respiratory tract (76%), breast(33%), kidney, urinary, digestive tract and unspecified (63 %) p value=0.001; and the means PTHrP(Normal<2.5pmol/l) was low in hematological malignancies as compared to the rest.[6] Cases of hypercalcemia with low PTH and PTHrp in patients of ALL have been reported very rarely.[7] After laboratory confirmation of hypercalcemia, serum albumin levels are measured for the interpretation of actual serum calcium level; in case albumin levels are abnormal, then corrected calcium needs to be calculated by the formula (serum calcium [mg/dL] + 0.8 × (normal albumin – serum albumin [g/dL]) and besides electrocardiogram (ECG) should be taken and corrected QT interval should be calculated to look for QT shortening. As in this case, serum albumin was normal, so serum calcium was taken as such, and ECG showed QT shortening. The initial treatment for hypercalcemia is intensive hydration and diuretics. If this treatment fails, corticosteroids may be useful.[8] Loop diuretics (e.g., furosemide) may be used after correction of dehydration, with strict fluid and electrolyte monitoring to augment urinary calcium excretion further.[9] An alternative therapy is the administration of bisphosphonates, which are very powerful inhibitors of bone resorption.[10] In our case, hypercalcemia was treated with intensive hydration, furosemide and bisphosphonates. The patient was then referred to a higher haematological centre for chemotherapy.
CONCLUSION
Our case demonstrates that hypercalcemia unveiled leukaemia in an adult, and so ALL should be considered as one of the differential diagnoses in a young adult presenting with incidental hypercalcemia. And that hypercalcemia with low serum PTH and serum PTHrp suggested haematological malignancy. Peripheral blood smear and bone marrow should be advised early by suspecting leukaemia.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Acute Lymphoid Leukemia In: Harrisson’s Principals of Internal Medicine (21st ed). United States: McGraw-Hill; 2022. p. :828-30.
- [Google Scholar]
- Disorders of Parathyroid Gland and Calcium Homeostasis In: Harrisson’s Principals of Internal Medicine (21st ed). United States: McGraw-Hill; 2022. p. :3169-83.
- [Google Scholar]
- Hypercalcemia in Children Presenting with Acute Lymphoblastic Leukemia. Int J Hematol. 1997;66:353-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hypercalcemia Complicating Childhood Malignancies: A Report of Seven Cases with Some Pathophysiological Considerations. Cancer. 1979;44:2280-90.
- [CrossRef] [PubMed] [Google Scholar]
- Hormones and Disorders of Mineral Metabolism In: William's Textbook of Endocrinology (14th ed). Philadelphia, PA: Elsevier; 2020. p. :1196-210.
- [Google Scholar]
- Serum Parathyroid Hormone-Related Protein Levels and Response to Bisphosphonate Treatment in Hypercalcemia of Malignancy. J Clin Endocrinol Metab. 1999;84:3545-50.
- [CrossRef] [PubMed] [Google Scholar]
- PTHrP-Independent Hypercalcemia with Increased Proinflammatory Cytokines and Bone Resorption in Two Children with CD19-Negative Precursor B Acute Lymphoblastic Leukemia. Pediatr Blood Cancer. 2007;49:990-3.
- [CrossRef] [PubMed] [Google Scholar]
- A Case of Acute Lymphoblastic Leukemia Presenting as Severe Hypercalcemia. Pediatr Hematol Oncol. 2004;21:475-9.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment and Management of Patients with Abnormal Calcium. Crit Care Med. 2004;32:146-54.
- [CrossRef] [PubMed] [Google Scholar]
- Use of Bisphosphonates for Resistant Hypercalcemia in Children with Acute Lymphoblastic Leukemia: Report of Two Cases and Review of the Literature. Turk J Pediatr. 2006;48:248-52.
- [Google Scholar]







